Service Definitions is the foundation for setting up services that providers treating clients use as criteria to apply charges that are consistent and acceptable to payers. Service Definition configurations flow through all claim and billing processes. Accurate entry of component details to uniquely identify each Service Definition is essential during setup to avoid Service Entry and Fiscal Overview Functions errors as billing procedures are performed. Selecting Service Definitions under Services/Payers in the Configuration menu displays the search bar and add icon (blue plus "+").
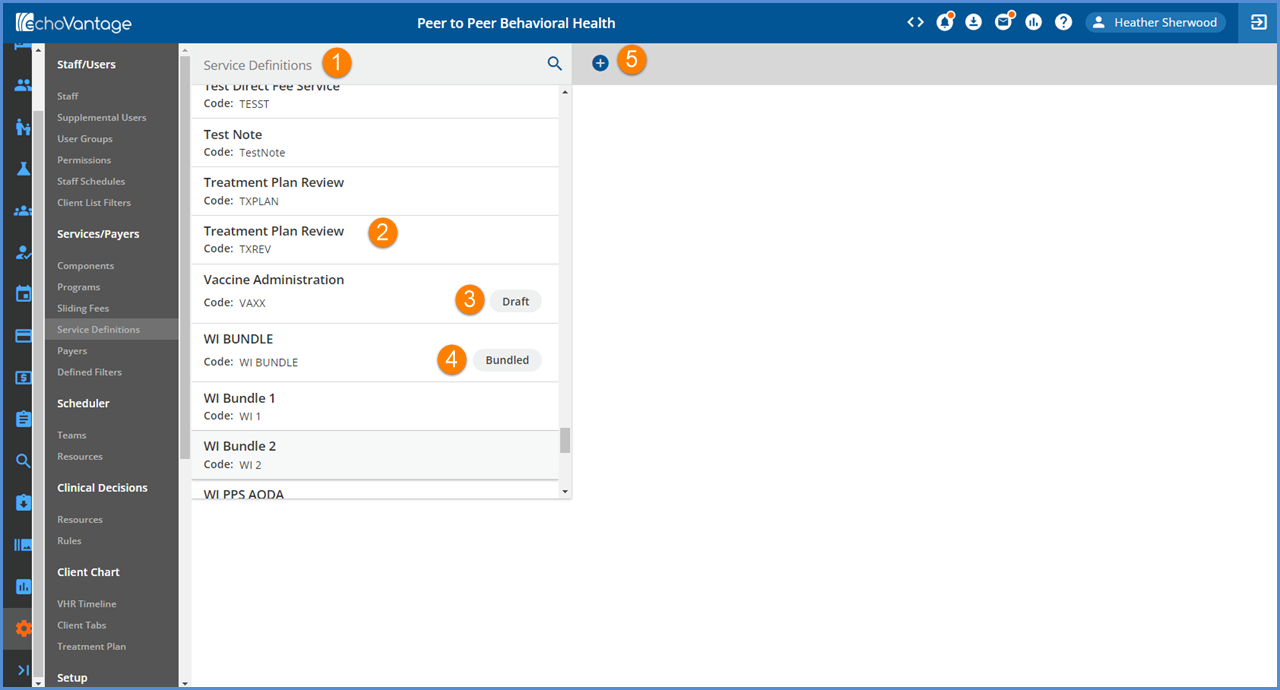
1. An existing Service Definition may be located by typing any portion of the code or description in the search bar.
2. The list below filters down to the best or complete match.
3. Service Definitions that are not yet published have a Draft indicator.
4. Bundled Service Definitions have a Bundled indicator.
5. Select the blue plus (+) to the right of the search bar to add a new Service Definition.
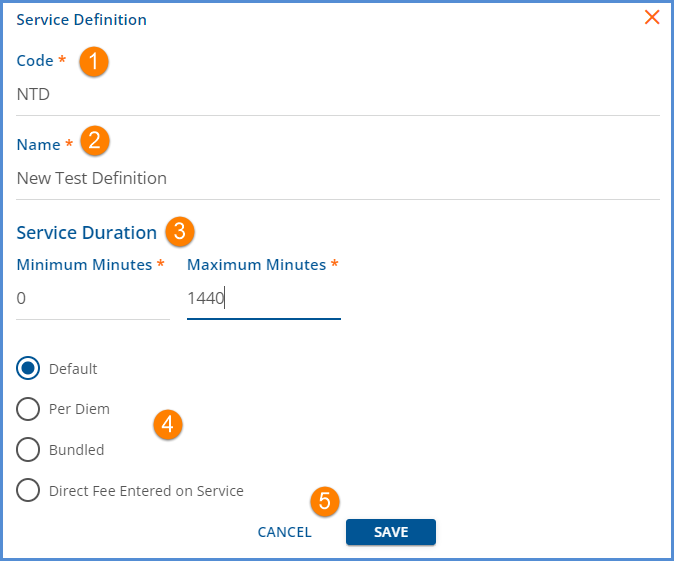
1. Code - Code is a required, free text field with a maximum of 10 characters.
2. Name - Name is a required, free text field with a maximum of 30 characters. Use to further identify the Service Definition; this name is displayed on the Service Entry screen.
3. Service Duration - The Minimum and Maximum minutes are required for all Service Definitions and define the Service Duration.
- Minimum Minutes must be less than the Maximum Minutes.
- Durations under Rates are used in processing to check those rates when determining if a charge can be calculated for a payer.
- Rates durations can continue to be set on the Rates tab if billing durations differ from the acceptable durations entered during Service Entry.
- For example, if a Service can be entered for any duration but is only billable if the service lasts at least 8 minutes. 1 minute would be entered as the Minimum duration on the Profile tab and 8 minutes as the Minimum duraton on the Rates tab.
- CPT codes for the same service that vary based on time can be assigned to the appropriate Service Definition configuration and will be applied correctly in billing.
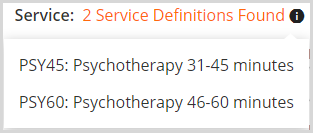
- **NOTE** The Service Duration for the same Activity code (component combinations) cannot overlap.
- The durations must be exclusive of each other for a unique Service Definition to be applied.
- When the ranges overlap, a warning message is displayed indicating that multiple Service Definitions have been found.
-
4. Type of Service Definition - Select a radio button to indicate the type of Service Definition being created. Use care to make the correct selection as the Service Definition type CAN NOT be changed after the Service Definition is saved AND published.
- Default - Default is the standard type of Service Definition. It can have rates defined, is not considered in Per Diem billing, and does NOT bundle.
- Per Diem - Per Diem Services are used to calculate date range services.
- Units for Per Diem services are pulled from the date range, one unit per day.
- In contrast, units are calculated for a default service based on the Unit Calculation and Minutes per Unit settings defined.
- Bundled - Select Bundled if the service definition is for a bundle of services. Bundled service definitions have additional configuration options.
- Direct Fee Entered on Service - Select this option when the charge amount is dependent on factors other than rate and unit.
- The amount for a Direct Fee is directly entered on the Service Entry screen.
- For Clinician's Desktop users, Direct Fee replaces the Standard Charge field in Activity entry.
5. Select SAVE to add the Service Definition to the list. Select CANCEL to exit the add Service Definition screen without saving.
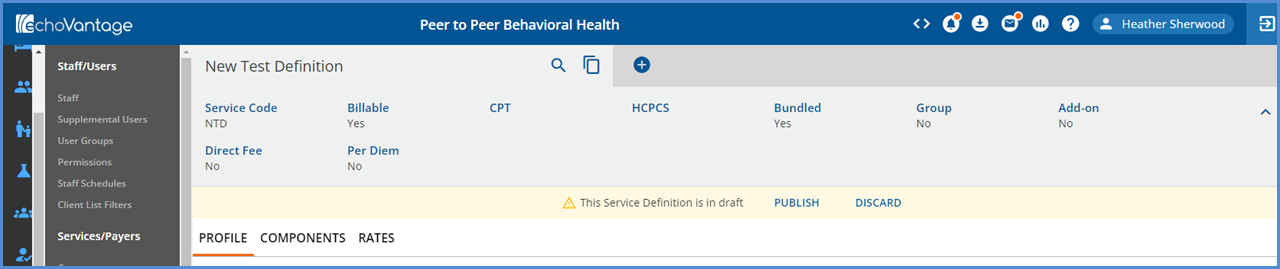
- Newly saved Service Definitions are created in DRAFT status, as indicated by the yellow warning banner.
- Service Definitions remain in DRAFT status until they are either published or deleted.
- Only published Service Definitions are considered on the Service Entry screen.
- Selecting DISCARD deletes the Service Definition Draft from the list, from any Bundled Service Definitions, and deletes any Payer Overrides for that Service Definition.
- The grey header contains summary information like: Service Code, Billable, CPT, HCPCS, Bundled, Group, Add-On, Direct Fee, and Per Diem.
- As entries are made on the Service Definition's tabs, these labels are populated.
- A Bundled Service Definition has three tabs: Profile, Components, and Rates.
- In the image above, Profile is the currently selected tab as indicated by the orange horizontal bar.
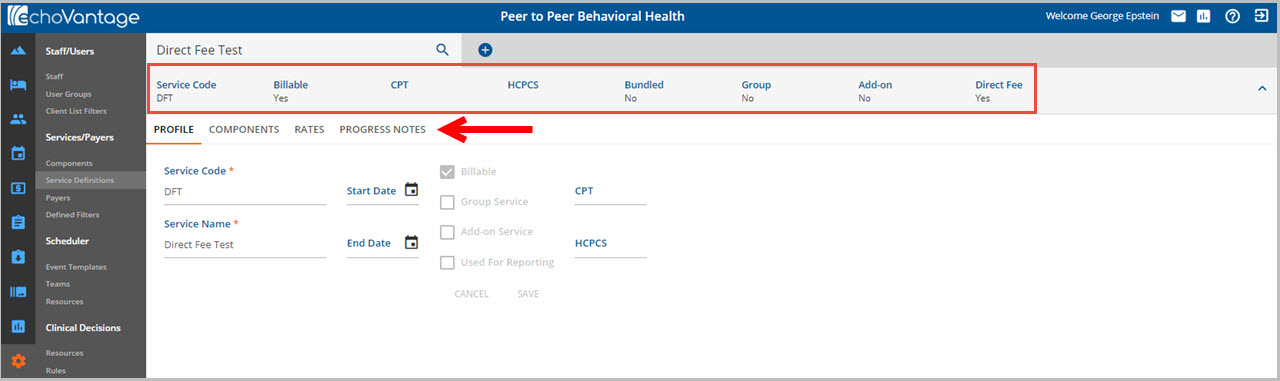
A non Bundled service definition has four tabs: Profile, Components, Rates, and Progress Notes.
