Configuring the CMS-1500 Paper Billing Method
The CMS-1500 Paper Billing Method is used by all licensed healthcare providers to bill all medical insurances including Medicare, Medicaid, and Blue Cross. Form CMS 1500 is formerly known as HCFA 1500 form and is also known as the universal claim form. Starting with the release of version 3.25 the CMS 1500 Configuration screen is divided into Payer Options and Reporting Options columns. Fields are clearly labeled, the CMS 1500 paper form box numbers are referenced in the Reporting Options, and presented in the Box number order to take the guesswork out of the setup. A brief description of each field is listed beneath the sample image below. Start by navigating to Configuration > Services/Payers > Payers > Billing Methods > CMS-1500 Paper.
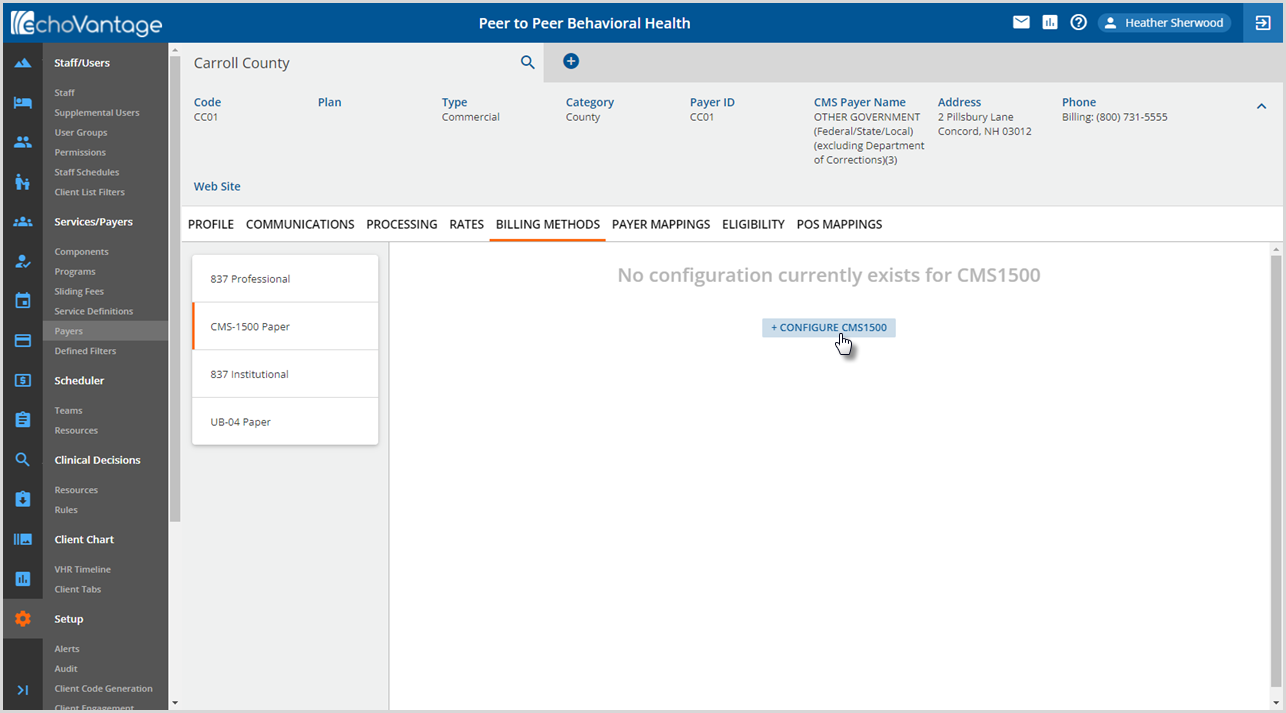
Click on + CONFIGURE CMS1500 to open the CMS 1500 Configuration screen to open the configuration screen.
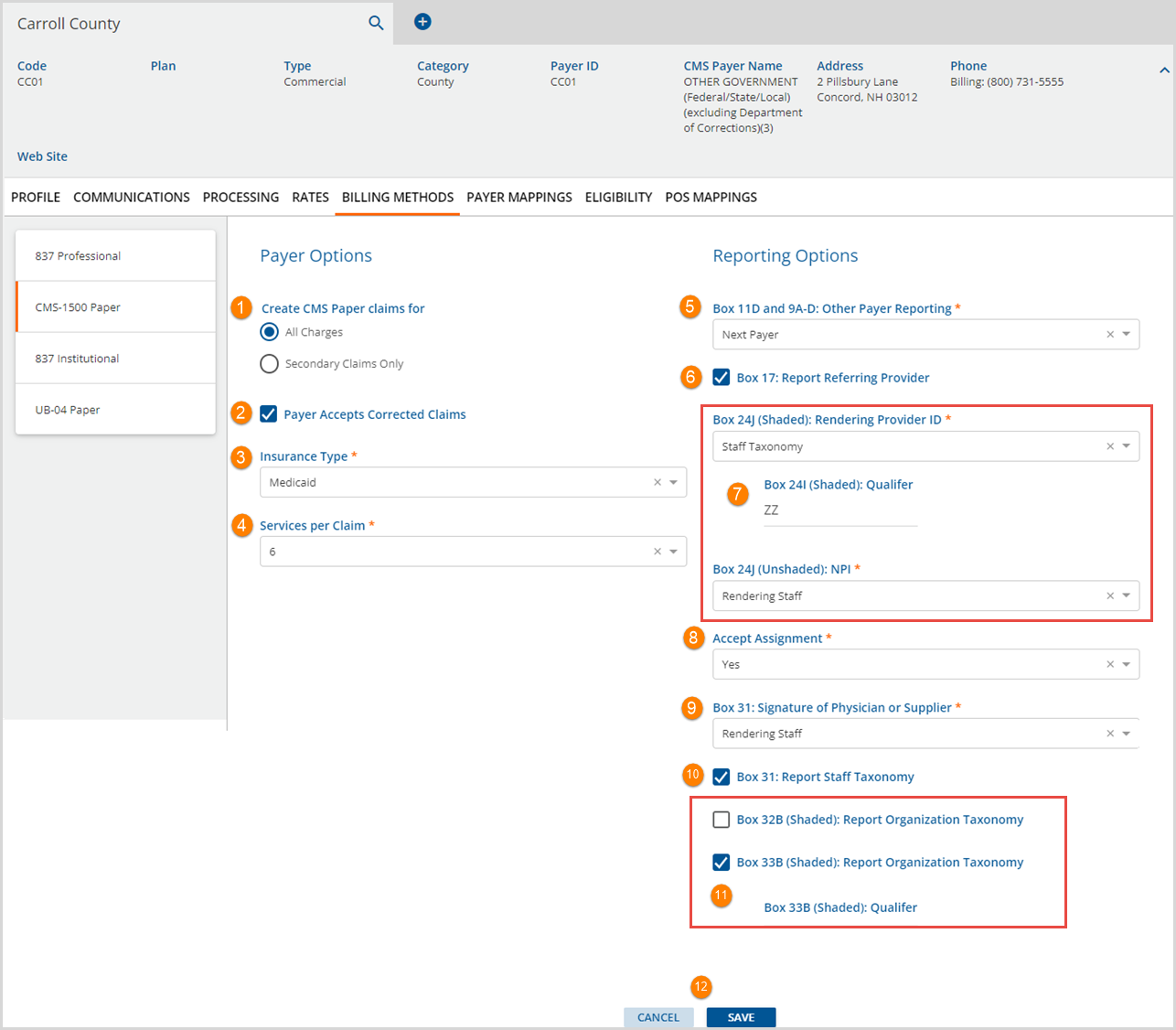
Payer Options
1. Create CMS Paper claims for - All Charges or Secondary Claims Only are available to select. Selecting one automatically deselects the other.
2. Payer Accepts Corrected Claims - Select the checkbox if the payer accepts corrected claims.
- A corrected claim is identified as already having a payment (a zero payment in the case of a denial or a positive payment in the case of an accidental payment) from the payer being billed.
- When reprocessing or rebilling using the CMS-1500 billing method and the claim is a corrected claim and the Payer Accepts Corrected Claims checkbox is selected:
- If the payment has a PCCN,
- Box 22 Resubmission Code = '7'
- Box 22 Original Submission Code is the PCCN from the prior Payment
- If there is no PCCN,
- An error is logged during bill creation.
- And a CMS-1500 is created that only contains corrections.
- If the payment has a PCCN,
3. Insurance Type - Use the drop-down list to select the Insurance Type. These correspond to the checkboxes in Box 1 of the paper CMS 1500 form. The drop-down list values available for selection are:
- Medicaid
- Medicare
- Tricare
- CHAMPVA
- Group Health Plan
- FECA BLK Lung
- Other
4. Services per Claim - Values of 1-6 are available for selection in the drop-down list.
Reporting Options
5. Box11D and 9A-D: Other Payer Reporting - Selection values of Next Payer or Prior Payer are available.
- The following is reported for the Payer currently being billed.
- Box 11: Client Payer Policy Number
- Box 11a: Subscriber’s date of birth and Male or Female checkbox selected
- Box 11c: Client Payer Policy Name
- Box 11d: The checkbox has an X if there is a Client Payer with a higher priority
- The following is reported based on the selection of either Next Payer or Prior Payer.
- Box 9a: Next or Prior Payer’s Client Payer Policy Number
- Box 9d: Next or Prior Client Payer’s Name
6. Box 17: Report Referring Provider - Select the checkbox if Referring Provider is to be reported. Referring Provider information is pulled from the Referrals grid on the Clients>Enrollments tab based on the following criteria.
- If the Client has no Enrollments, a "Referring Provider Missing" warning is reported.
- If a Client has Enrollments,
- And an Enrollment has a Start and End date that encompasses the Service Date AND the Enrollment Program matches the Service Program, the Referring Provider listed on that Enrollment is reported. If more than one Provider is listed, the highest priority Provider is selected.
- And an Enrollment cannot be matched to the Service Date, Service Program, or both, a "Referring Provider Missing" warning is reported.
- If the Report Referring Provider checkbox has not been selected, Box 17 is not populated.
7. Configuration for Box 24J is split between Shaded and Unshaded, and configuration for Box 24I is included in the Shaded section.
- Box 24J (Shaded): Rendering Provider ID – A selection is required and can be one of the following options.
- The following selection options are available in the drop-down list.
- Report Nothing - No value is reported in box 24J(Shaded).
- Staff Taxonomy - The Rendering Provider's Staff Taxonomy value from Configuration > Staff/Users > Staff > Profile is reported.
- Organization Provider Number - When selected, the value that matches the Defined Filter in Configuration > Services/Payers > Payers > Payer Mappings > Provider Numbers is reported. If nothing matches, it is left blank.
- The following selection options are available in the drop-down list.
- Box 24I (Shaded) Qualifier – When populated, the entered Qualifier is reported. If the Staff Taxonomy option is selected in Box24J(Shaded), the Qualifier defaults to ZZ but can be overridden.
- Box 24J (Unshaded): NPI – This required selection determines which NPI number to report, if any.
- The options available are:
- Report Nothing - No NPI information is reported in Box 24J.
- Rendering Staff - The Service Staff's NPI is reported.
- Supervising Staff - The Service Supervising Staff's NPI is reported.
- In addition, when the Staff person reported has a different NPI than another Staff on the Claim, the Services for the separate Staff are reported on a different claim form. The following scenarios outline what is reported for a Client with "ready to bill" Services from Rendering Staff 1 and Rendering Staff 2.
- The options available are:
|
Scenario 1
|
Scenario 2
|
|
Scenario 3
|
Scenario 4
|
8. Accept Assignment - A selection of either Yes or No is required. The default value is Yes and may be changed.
9. Box 31: Signature of Physician or Supplier - A selection of either Rendering Staff or Supervising Staff is required.
10. Box 31: Report Staff Taxonomy - The value reported is based on the selection in #9 above.
- If Rendering Staff is selected, the Staff Taxonomy code of the Service's (rendering) Staff is reported.
- If the Supervising Staff is selected, the the Staff Taxonomy code of the Supervising Staff is reported. If the Service does not have a Supervising Staff, the Rendering Staff Taxonomy code is reported.
11. Box 32B (Shaded) and Box 33B (Shaded) - The selection determines where the Organization Taxonomy code is reported, either Box 32B or 33B.
- Box 32B (Shaded): Report Organization Taxonomy -
- Box 33B (Shaded): Report Organization Taxonomy -
- Box 33B (Shaded): Qualifier - The organizational taxonomy 2-character qualifier value must be manually entered to populate Box 33B.
- There is no default value.
- If the Configuration > Organizations > Taxonomy field is null, this qualifier is not displayed in the CMS1500 Box 33B.
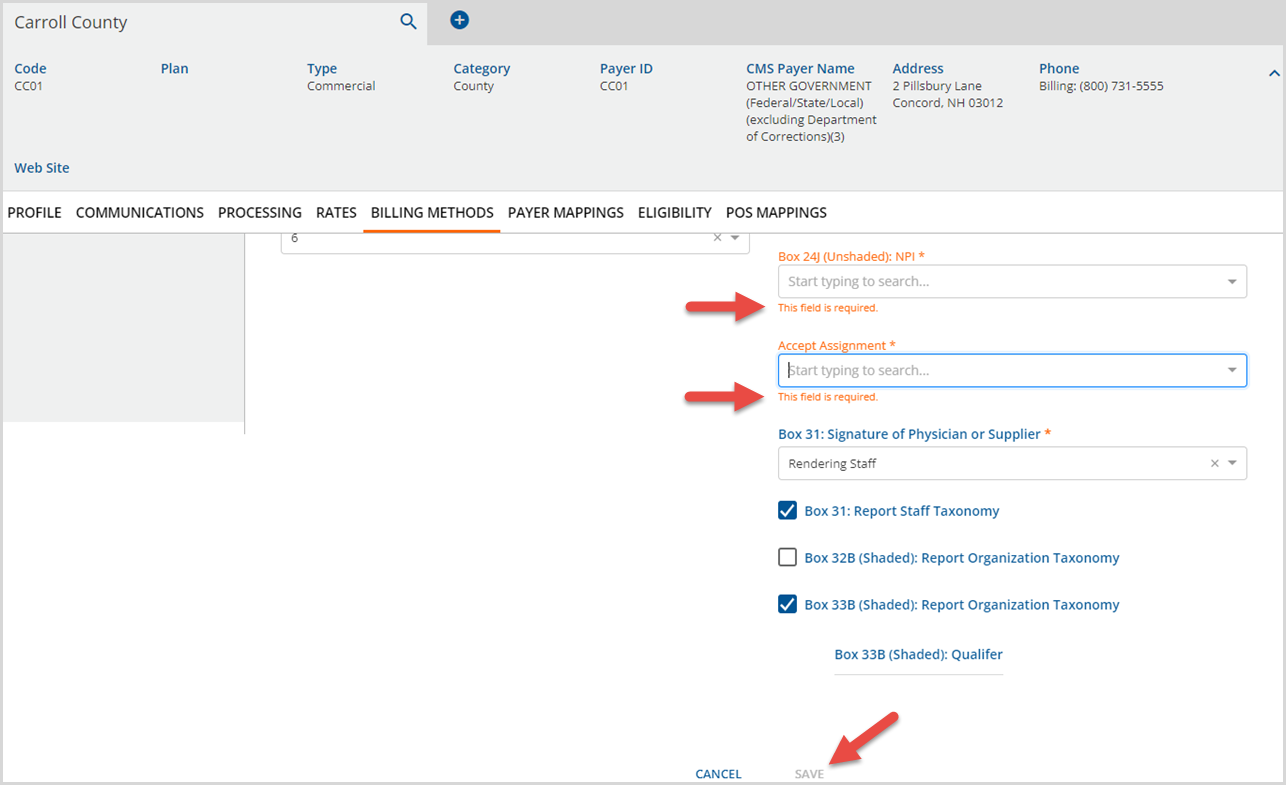
12. The blue SAVE button is enabled once all required fields are completed. Select SAVE to add the CMS-1500 Configuration or select CANCEL to exit without adding.
Please note that there is no configuration option and no value is reported, for any reason, in Box 24H.
Editing the CMS-1500 Form
Navigate to Configuration > Services/Payers > Payers > Billing Methods and select the CMS-1500 Form. The completed CMS-1500 Configuration displays. Click on any field to make the necessary edits. The blue SAVE is enabled again when the required fields are completed. If any required field is deleted and not repopulated, on-screen messages display, and SAVE is not enabled.