With the release of EchoVantage version 3.08, the Enrollments tab was redesigned to accommodate the additional fields needed to report the Referring Provider on the 837P. With the release of version 3.11, these same fields are used to populate the Referring Provider information on a CMS 1500 billing form when the "Report Referring Provider in Box 17" checkbox is selected on the CMS 1500 configuration. A completed Enrollments screen example is shown below and a short description for each field is included.
Click on the following links for detailed instructions for:
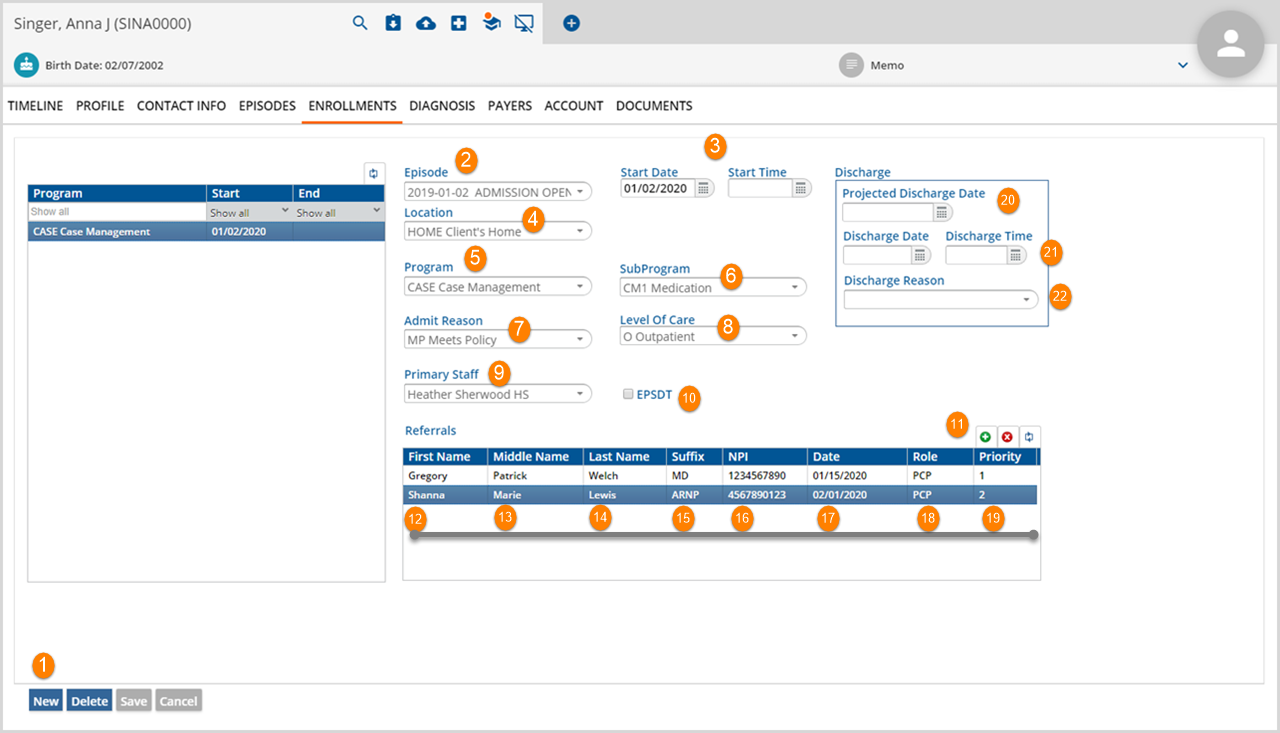
1. Select the blue New button on the bootm left of the Enrollment scren to add a new Client Enrollment.
2. Episode - Select the Episode from the drop-down list. This list is populated from the episodes entered on the Episodes tab.
3. Start Date/Start Time - These fields record the date the Enrollment began and the time the Enrollment began. The fields are not required.
4. Location - This drop-down list is populated with the Location codes and descriptions from the Location component. This field is not required.
5. Program - Select the Program for the current Enrollment from the drop-down list. Note that the Program grid to the left is updated with the Program and Start Date (and End Date if applicable) after the Enrollment is saved.
6. SubProgram - This drop-down list is populated with the SubProgram codes and descriptions for the selected Program if these were defined in Configuration>Services/Payers>Programs.
7. Admit Reason - Select the Admit Reason from the drop-down list. This list may be defined in Configurations>Setup>Defined Lists>Enrollment Admission Reasons *Contact your System Administrator if drop-down list values require changes.
8. Level of Care - Select the Level of Care for the current entry from the drop-down list. This list may be defined in Configurations>Setup>Defined Lists>Enrollment Admission Reasons *Contact your System Administrator if drop-down list values require changes.
9. Primary Staff - Select the Primary Staff from the drop-down list. This list is populated from the Staff grid on the Episodes tab. An Enrollment Primary Staff may differ from the associated Episode's Primary Staff.
10. EPSDT - (Early and Periodic Screening Diagnosis and Treatment) Check this box if the Client receives comprehensive and preventative health care to the maximum extent that Medicaid allows. The ANSI 837 billing format and others require this information.
11. Clicking the green (+) will save any Enrollment information just entered, updating the Program grid if applicable and allowing entry into the fields in the grid beneath it. This grid has 6 additional input entry fields to capture the required information for reporting the Referring Provider on the 837P or the CMS 1500.
12. First Name - The referring provider first name.
13. Middle Name - The referring provider middle name.
14. Last Name - The referring provider last name.
15. Suffix - The referring provider suffix.
16. NPI - Enter the referring provider's 10 digit unique identifying number issued by the Centers for Medicare and Medicaid Services
17. Date - Use the down arrow to display a calendar and select the date of referral.
18. Role - Role describes the Referred By by title. For example, a Referred By entry of Individual may have a role entry of Mental Health Therapist or Primary Care Physician.
19. Priority - This is a numerical field to prioritize the providers if there are more than one. The 837P or CMS 1500 will take the highest priority provider that is active during the Service date.
20. Projected Discharge Date - This is the anticipated date of discharge for the Enrollment. This field may be left blank.
21. Discharge Date and Discharge Time- This is the actual date and time of discharge for the Enrollment. The Enrollment Discharge Date must fall within the associated Episode's date range. If a discharge date is entered, it will populate the End date in the Program grid once the entry has been saved.
22. Discharge Reason - Select the Discharge Reason from the drop-down list. This list is defined in Configurations>Setup>Defined Lists>Enrollment Discharge Reasons. *Contact your System Administrator if drop-down list values require changes.
Click on any field (2-10, 20-22) in the current Enrollment to edit. Double click a field in the Referrals grid to modify that record. The blue Save button will be enabled when all required fields are populated or if changes are made to an existing Enrollment.
**NOTE**
Care Plan referrals will not be picked up and reported on the 837P. Referrals must be entered through the Enrollments tab to be included in the billing file.
Referring Provider in the 837P or CMS 1500
The following criteria is evaluated if the CMS 1500 Report Referring Provider in Box 17 or the 837P Report Referring Provider (Loop 2310A) checkbox has been selected in the Payer Billing Method configuration:
- If the Client has no Enrollments, a "Referring Provider Missing" warning is reported.
- If a Client has Enrollments,
- And the Enrollment has a Start and End date that encompasses the Service AND the Enrollment Program matches the Service, the Referring Provider listed on that Enrollment will be reported. If more than one Provider is listed, the highest priority Provider will be selected.
- And no Enrollments can be matched to the Service, a "Referring Provider Missing" warning is reported.
- If the Report Referring Provider checkbox has not been selected,
- Box 17 will not be populated or
- Loop 2310A will not be present.
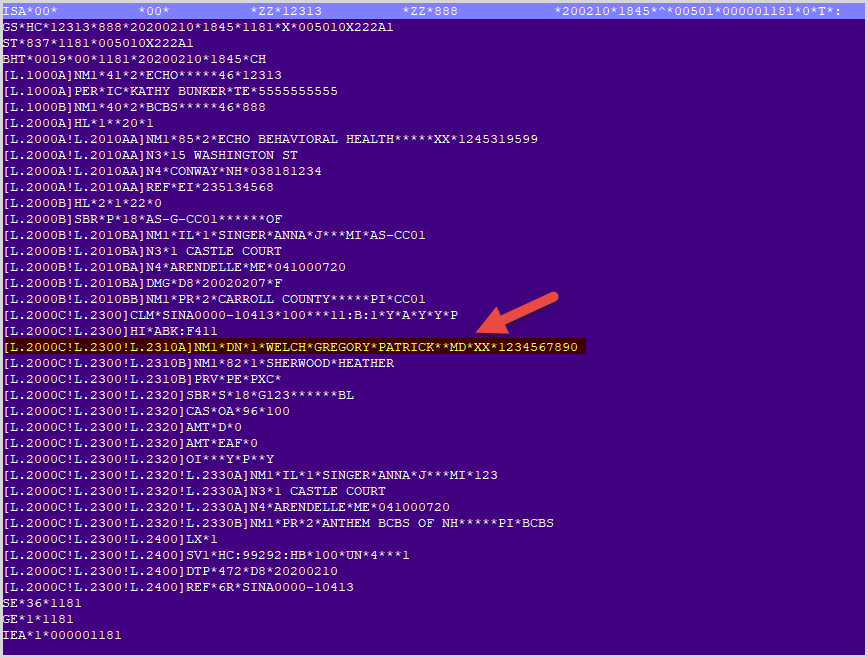
The 837P example below shows a Service that was billed with that matches on the Enrollment example shown above.