The Eligibility REQUESTS screen contains a row for each client’s eligibility requests. The list is sorted to display the most recent eligibility requests first, grouped by Payer.
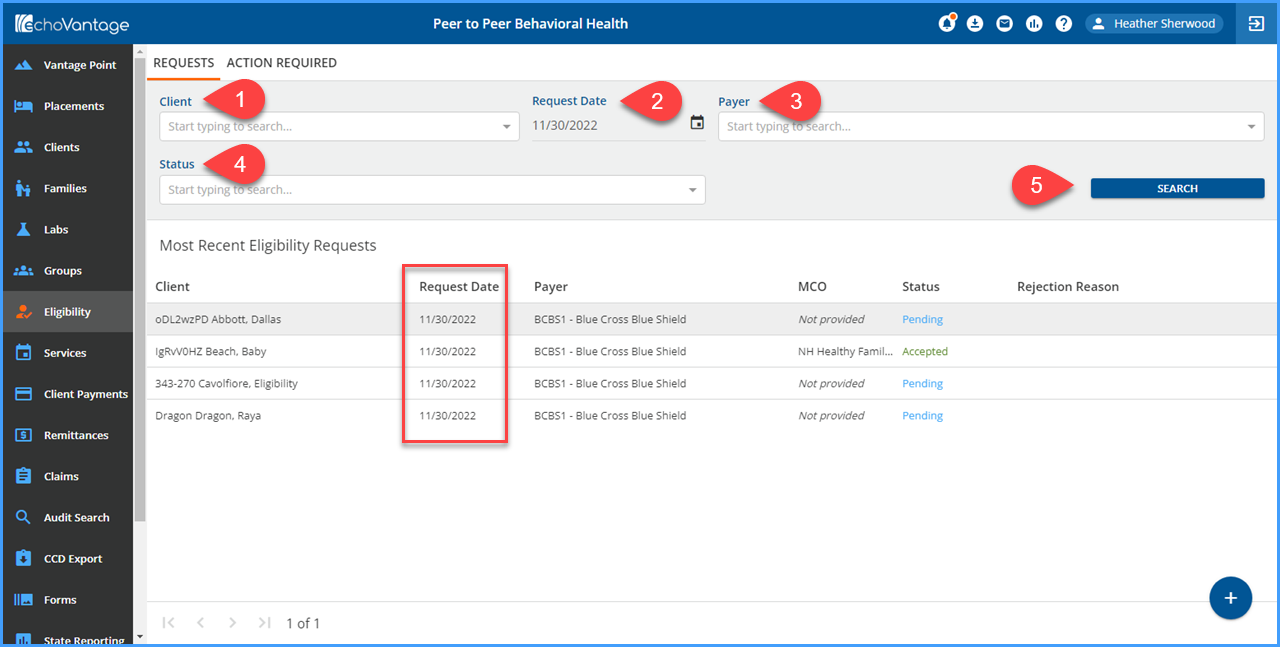
The grey header area contains filter fields to help locate a specific client requests or groups of requests.
-
Client - Allows the user to select and search for a specific client.
-
Request Date - Allows the user to locate client requests records created on a specific date. In the example above, the results are limited to just requests created on 6/20/2019. Note that both Anthem and Medicaid are listed as Payers.
-
Payer - Allows the user to search and filter the client request records base on Payer.
-
Status - Allows the user to search and filter based on the request status. All requests are initially Pending. Once a 271 file is imported, Accepted and Rejected will be available to user for filtering.
-
SEARCH - The blue Search button is used to execute the Search once the selections have been made. Any combination of 1 through 4 may be used to drill down to the desired request or requests.
In the example above, only requests dated 11/30/2022 are displayed which makes for a much more manageable group of requests to work with and view. Once requests are either Accepted or Rejected, the Eligibility Details may be viewed or there will be a Rejection Reason.
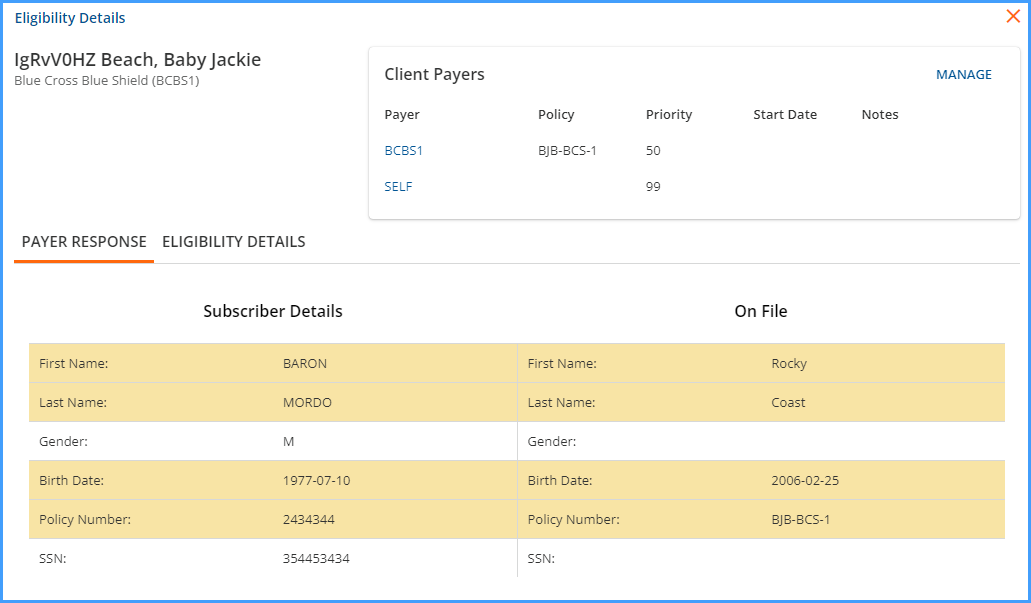
Clicking on the word Accepted opens the Eligibility Details screen.
-
The selected client’s name and the eligibility response payer are displayed in the top left corner.
-
There are two tabs to the screen: Payer Response and Eligibility Details. The orange horizontal line indicates the current selection.
-
The Subscriber Details section displays the information from the Payer’s response and the On File sections displays summary information from the Client's Profile and Payers tab. Discrepancies are highlighted.
-
The Client Payers section list the Payers that are currently associated with the client.
-
The Manage button in the Client Payers section links directly to the Client's Payers screen so that changes or updates may be made.
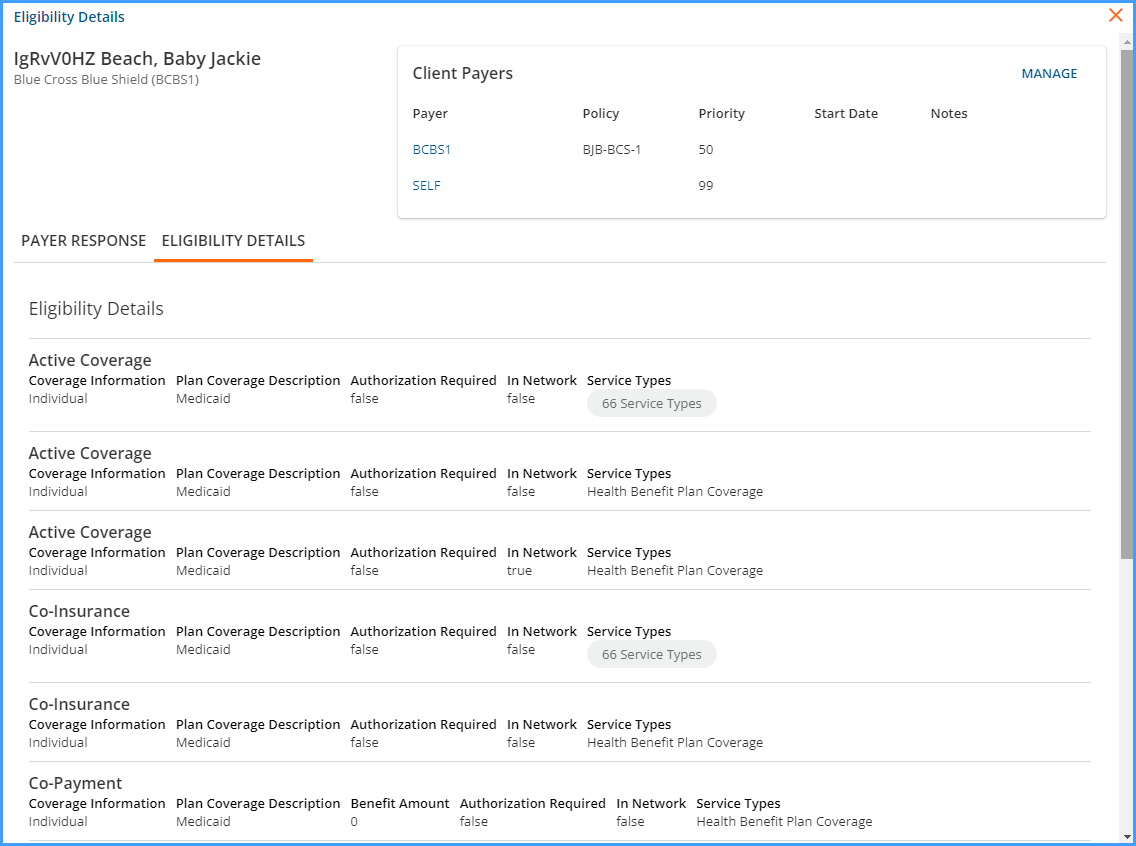
Selecting Eligibility Details displays the Coverage and Service Type details.
Just like the Payer Response screen:
-
The upper left-hand corner has the client name and the eligibility response payer.
-
Client Payers displays a list of Payers already associated with the client.
-
Manage links directly to the client’s Payers screen to add, edit, or delete information as needed per the Payer response.
If Eligibility Details pertain to different Service Types, click the Service Types button to view the list. The number indicates the tally of the eligible types. Clicking on the button displays the following:
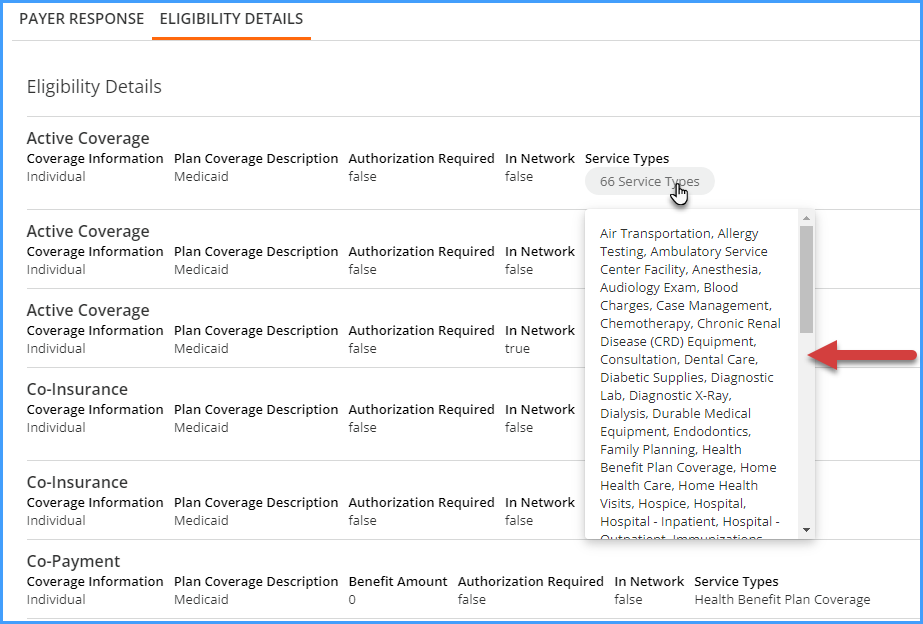
When finished viewing the client request record, use the red "x" in the upper right-hand corner to exit the Eligibility Details screen.
